
Dementia poses a major global health challenge, with an estimated increase in the number of people living with dementia from 57.4 million in 2019 to 152.8 million by 2050. Proactive management of modifiable risk factors such as hypertension is pivotal in dementia prevention. While the correlation between elevated blood pressure (BP) and dementia is well-established, there are still no proven interventions that prevent or delay the development of dementia [1]. However, a recent trial aimed at BP lowering showed that the intervention not only reduced BP but also significantly reduced the risk of total dementia [1,2].
A study by Jiang He et al., presented in the “American Heart Association Scientific Sessions 2023”, reported that BP lowering is effective in reducing the risk of dementia and cognitive impairment in patients with hypertension over a 48-month intervention period [2].
This open-label, blind-endpoint, cluster-randomized study involved 33,995 individuals aged 40 years and older from 326 villages. Participants included in the study had untreated BP ≥140/90 mmHg, and a history of cardiovascular disease, chronic kidney disease, or diabetes. During randomization, 163 villages each were allocated to the intervention group and the usual care group. The intervention followed a stepped-care protocol for hypertension treatment. The goal was to achieve a target systolic BP of <130 mm Hg and diastolic BP of <80 mm Hg. Village doctors initiated and adjusted antihypertensive treatment based on the protocol. Health coaching on lifestyle modification and medication adherence was conducted. Patients were instructed on home BP monitoring. The primary outcome was all-cause dementia, and the secondary outcomes were adjudicated cognitive impairment and a composite outcome of dementia or cognitive impairment. All clinical events, including cognitive outcomes and mortality, were independently adjudicated by two neurologists who were blinded to the intervention assignments [1,2].
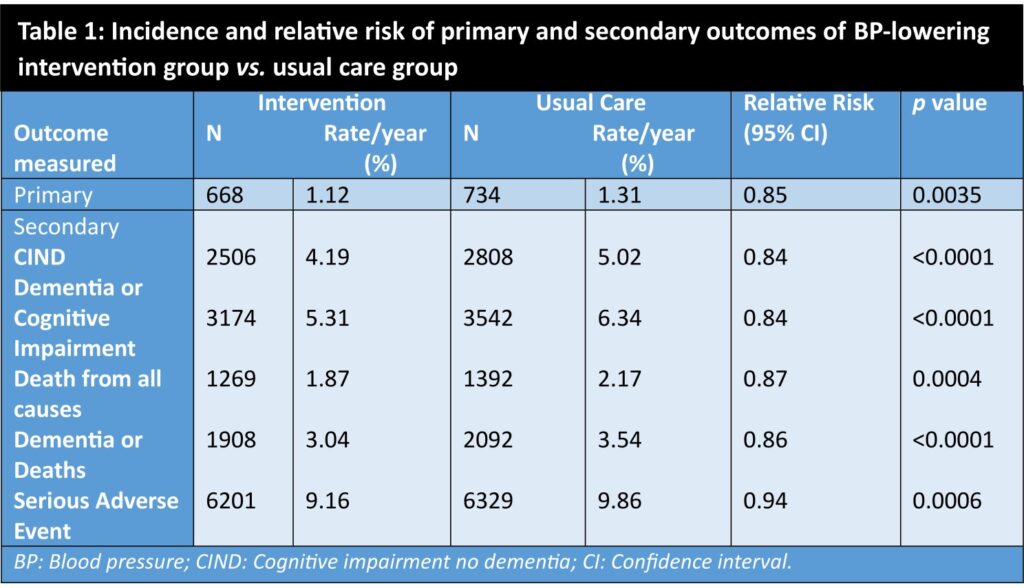
The study results are summarized below [1]:
- At 48 months, the mean systolic/diastolic BP in the intervention group was 127.6/72.6 mm Hg compared to 147.7/81 mm Hg in the usual-care group.
- The net change in systolic BP was ─22.0 mm Hg (95% CI -23.4 to -20.6; p <0.0001), and that of diastolic BP was ─9.3 mmHg (-10.0 to -8.7; p <0.0001).
- The primary outcome of dementia occurred at a rate of 1.12% per year in the intervention group compared to 1.31% per year in the usual-care group (Figure 1 and Table 1). Intervention led to a relative risk reduction by 15% (relative risk with the intervention was 0.85; 95% CI: 0.76 to 0.95, p = 0.0035).
- The endpoint of cognitive impairment and composite outcome of dementia or cognitive impairment were lower in the intervention group compared to the usual-care group (Table 1).
- The composite outcome of dementia or deaths were both significantly lower in the intervention group compared to the usual-care group (Table 1).
Clinical implications [1,2]
- This study findings suggest that actively managing and achieving lower blood pressure levels (systolic BP <130 mmHg and diastolic BP <80 mmHg) through a stepped-care protocol can contribute to a reduced risk of dementia and cognitive impairment.
- Incorporating such interventions into routine healthcare practices could be instrumental in addressing cognitive health issues, particularly in populations with untreated hypertension.
- The study underscores the importance of a comprehensive approach to hypertension management, extending beyond the conventional medical setting, and highlights the potential for substantial public health benefits with reducing the burden of dementia and cognitive decline.
(References: 1. Jeffrey S. Blood pressure lowering reduces dementia risk. Medscape [Internet]. 2023 [cited 2023 Nov 16]. Available from: https://www.medscape.com/viewarticle/998381 2. He J; Zhao C; Zhong S, et al. Effectiveness of blood pressure-lowering intervention on risk of total dementia among patients with hypertension: A cluster-randomized effectiveness trial. American Heart Association (AHA) Scientific Sessions 2023. Presented November 11, 2023)
